I was shocked to read a news release from the Oregon Department of Human Services and Oregon Health Authority issued on March 3, 2023. Oregon will lift mask requirement for health care settings April 3 (govdelivery.com).
The title of the memo is “Oregon will lift mask requirement for health care settings April 3.”
There are many problems with this decision. I would put my objections to it in two categories. The first category concerns matters upon which reasonable persons can disagree, but if you are going to take a position, at least make logical and internally consistent arguments to support your position and decision. The other category involves the fact that this decision is coming from a government agency charged with protecting the health of Oregonians, and yet there is no discussion as to how this decision serves the people of Oregon.
Let’s start with what the Oregon Health Authority’s purpose is:
Oregon Health Authority (OHA) – on its website (https://www.oregon.gov/oha/pages/portal-about-oha.aspx), the vision of OHA is “a healthy Oregon.” The mission is “Ensuring all people and communities can achieve optimum physical, mental and social well-being through partnerships, prevention and access to quality, affordable health care.”
Now, let’s examine the memo to see if the action being taken is consistent with the agency’s vision and mission and determine whether the termination of the rule is supported by the resolution of the concerns that prompted the rule.
The memo states that the mask requirement will end for workers, patients and visitors beginning April 3 in all health care settings, rescinding Oregon Administrative Rule (OAR) 333-019-1011.
The memo states: “Dean Sidelinger, M.D., M.S.Ed., health officer and state epidemiologist at OHA, said the lifting of Oregon’s health care mask requirement stems from data in recent weeks showing overall decreases in circulation of the three respiratory pathogens that triggered a surge in visits to hospital emergency departments and intensive care units last fall.”
So, let’s just look at the first argument – “data in recent weeks showing overall decreases in circulation of the three respiratory pathogens (SARS-CoV-2, RSV and influenza) that triggered a surge in visits to hospital emergency departments and intensive care units last fall.” But this action rescinds the administrative rule cited above. So, let’s review the language of that rule Oregon Secretary of State Administrative Rules. Here are the key provisions of that rule for purposes of this issue:
- “This virus (SARS-CoV-2) can be spread by infected persons without symptoms as well as those with symptoms.”
- The rule also mentions that successive variants have developed an increase in transmissibility in the face of waning vaccine effectiveness.
- “Consistent masking by health care providers in health care settings, as well as masking by visitors and patients provides protection to health care providers and to the people they care for. Masks act as source control if the provider has COVID-19 and provide a protective effect if a patient has COVID-19.”
Hopefully, you now see the first two logical flaws and inconsistencies in the argument for rescinding the rule – (1) the circulation of RSV and influenza were not among the reasons for the implementation of the rule, so the decrease in their circulation is irrelevant; and (2) a surge in visits to hospital emergency departments and intensive care units was not a reason for the implementation of the rule, so the fact that this most recent surge in visits has subsided is also irrelevant.
If we look a bit closer at the argument provided by OHA, the only part of this first argument for terminating the rule that is applicable to the reasons provided for implementing the rule is the fact that “data in recent weeks showing overall decreases in circulation (of SARS-CoV-2).” Let’s see how strong that argument is.
Here is the most recent epi curve for Oregon from the CDC:
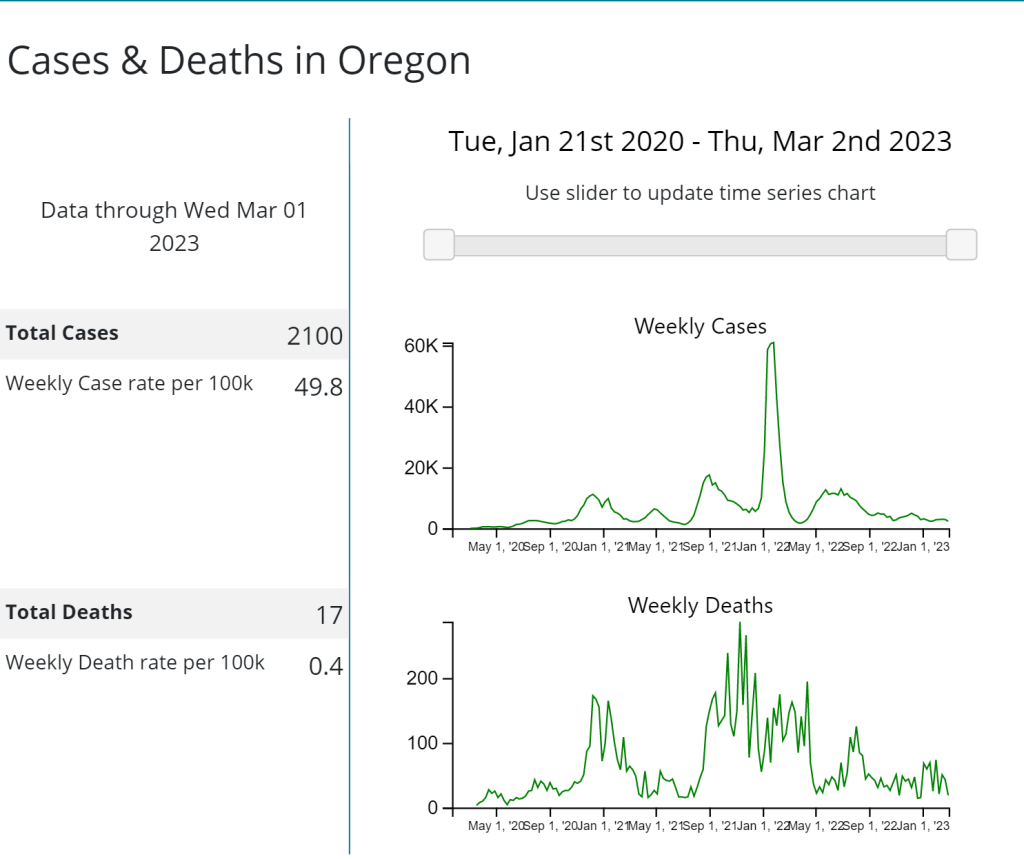
Again, the argument for terminating the rule is: “data in recent weeks showing overall decreases in circulation (of SARS-CoV-2).” This is actually at least the seventh time since the beginning of the pandemic that this same statement could be made. On each of the prior six occasions, that decrease was followed by a subsequent increase in cases, often by a significant surge in cases. So, why terminate it now and what makes OHA think that there won’t be another surge? Also, not addressed is the fact that we know testing has significantly decreased. Many people are no longer testing when they get sick and many others are testing at home. The results of at-home tests do not show up in the publicly reported numbers of cases. The lack of complete reporting of cases has increased the importance of wastewater testing. The CDC’s wastewater surveillance reporting indicates that 3 testing sites in Oregon are reporting levels of SARS-CoV-2 detection in the range of 60 – 79% of the highest levels reported during the pandemic – hardly an indication that SARS-CoV-2 transmission is under control.
Let’s look at the next argument in the memo: “As of today, COVID-19 test positivity is at 10% and is expected to continue dropping.” First of all, the fact that testing positivity is at 10% is not reassuring. For those who follow this kind of data, you will recall that the goal is for testing positivity to be less than 5%. Thus, the current testing positivity rate cannot be a strong argument for terminating the rule. Rather, OHA’s argument must rely on their assertion that the testing positivity rate “is expected to continue dropping.” It is odd then, that if that is the strongest point of OHA’s argument relating to testing positivity, it offers no explanation as to why it is expected to continue dropping, and especially why OHA has confidence that the testing positivity will continue dropping or be at a low level in a month, when the rule is to be terminated. With the occasion of the first recombinant becoming the predominant circulating variant in the US that also appears to be more transmissible and more immune evasive than prior variants and with a significant rise in the detection of new recombinants emerging, what possible evidence would suggest that we can expect significantly lower transmission rates in the future? I would be delighted if that were the case, but I wouldn’t be placing any bets on that.
The next argument made is that the month-long notice of the termination of the rule allows health care providers adequate time for ”adjusting policies, training and procedures that ensure continued patient safety.” I am curious as to what changes OHA thinks health care providers can take that will ensure patient safety with the ending of the mask requirement and studies that clearly demonstrate SARS-CoV-2 can be a hospital-acquired infection.
The next argument is that this advance notice also “gives members of the public, particularly populations at increased risk of severe disease—communities of color, tribal communities, rural communities, lower-income communities, those with underlying medical conditions, seniors, and parents of vulnerable infants – a chance to plan health care visits and protective measures.” This argument gave me the most visceral reaction. I have so many questions for OHA. What more exactly does it think that those members of the public that are at increased risk of severe disease (keep in mind that a large percentage of people who require outpatient hospital services and hospitalization will fit in this category) should do or can do if their caregivers are no longer masked? The memo goes on to offer a single recommendation: those who are at high risk or who live with persons who are at high risk should continue to mask. Wow. How is it that we are supposed to mask those “vulnerable infants?” If Dr. Sidelinger was going through aggressive chemotherapy, would he really feel safe being cared for in a hospital by an unmasked caregiver team? In a damning admission that this public health agency knows better, it admits that “Masks remain an effective way to reduce transmission of respiratory viruses.” What this statement leaves out is that the evidence is clear that transmission is further reduced when everyone sharing the same air is wearing high quality masks.
The last sentence of the memo is a correct statement: “In order to protect themselves and their families and communities, people are strongly encouraged to stay up to date with vaccinations and boosters.” But, it is an incomplete one. Current vaccines do a great job of protecting people from serious disease, hospitalization and death, if people are fully vaccinated, and have received the bivalent vaccine. In Oregon, only 72.44% of residents have completed the initial vaccination series. According to the CDC data, only 21.3% of Oregonians have received the updated bivalent booster. This large percentage of the population is less protected than they could be. While doing a fairly good job of protecting against severe disease, with the development of progressively more immune evasive variants, vaccines have been less effective at preventing transmission of infection. Further, while vaccines do reduce the chance for development of Long COVID, even vaccinated persons who get infected remain at risk.
I certainly am not suggesting that masking in health care settings will be necessary forever, simply that I think it is ill-advised at present, given the following facts:
- Transmission levels remain high. Despite OHA’s rosy projections, I think few experts feel comfortable in making any long-term projections as to how SARS-CoV-2 will continue to evolve and what threats it may pose.
- Variants have been evolving to achieve higher levels of transmissibility and higher levels of immune evasiveness. A general principle of epidemiology is that higher transmissibility requires more mitigation measures, not less if the objective is to lower infection rates.
- Vaccine effectiveness has declined.
- Insufficient numbers of citizens have been fully vaccinated and boosted, and large portions of the population are experiencing waning immunity either from vaccination or infection.
- Studies of long-term consequences of SARS-CoV-2 infection are revealing more concerns, not fewer.
- With a very limited exception, we no longer have effective monoclonal antibody treatment options due to the fact that current variants have developed progressively more degrees of immune evasion.
- We previously could offer immunocompromised patients and patients with immunodeficiencies Evusheld as protection against infection. However, as with the monoclonal antibodies, current variants have also developed immune evasion to this therapy.
Of course, the good news is that while the rule will terminate, hospitals and other facilities and caregivers who care for high-risk patients are not required to end their mask requirements. This rule change will make it more difficult for those providers to continue requiring masking, but I encourage them to do so for now for the following reasons:
- Evidence-based care: The provision of health care services should be evidence-based in those cases where evidence exists. Masking in health care settings remains evidence-based at present.
- Trust: There has, in general, been a decline in levels of trust for health care providers during the pandemic for many reasons, including the promotion of disinformation and conspiracy theories by legislators, and unfortunately, by some physicians and even members of health boards. We must act in ways that assure the public that we have their best interests at heart and they do not have to fear that they are safer in their homes than in our hospitals.
- Ethics: A long-held principle for physicians, but one generally applicable to health care is primum non nocere (first, do no harm). When patients come to us for help, we are obligated to act in their best interests (not ours), and certainly, it is expected that we will do our best to keep them safe while in our care.
- Workforce issues: During the pandemic, there have been points at which capacity has been strained. But, throughout this time, there have been pressures on adequate staffing given employees quarantining due to exposure or isolating due to infection. We continue to experience health care professional shortages. While acute infections add to these short-term staffing challenges, we are only now learning about the health risks associated with repeated infections and with Long COVID. At a time when hospital finances are strained for most hospitals, it hardly seems prudent to increase the needs for travelers, decrease the capacity to treat patients, increase employee health care costs, and lose more employee productivity due to Long COVID.
One of the most heartbreaking revelations of the pandemic has been the general apathy towards protecting those who are immunocompromised. I have talked to many elderly persons, parents taking chemotherapy for cancer or immunosuppressive medications for autoimmune diseases or solid organ transplants, persons with immunodeficiencies and others who have felt that they have had to put their lives on hold and make extraordinary restrictions to their normal activities because the general populus has determined the need to protect their individual liberties takes priority. However, it is even more appalling when I see public health agencies or officials and health care providers failing to protect the immunocompromised.
I have talked to many of these immunocompromised individuals. They consider whether they are going to take the risks to go to the grocery store, get their hair done, or even go to the doctor’s office, and if so, how they will time their visit to minimize contacts with others. No doubt they have already put off many non-urgent health services. This change in masking could cause them to further avoid contacts with the health care system, and I fear, to the detriment of their long-term health.
Hospitals considering ending mask requirements would need to ask themselves how they would explain to a parent that their newborn contracted COVID-19 while in the hospital and is now ill. Keep in mind that these infants are not eligible for vaccination or most of the treatments authorized or approved by the FDA. They would be unable to answer what the long-term health consequences to that infant may be. Hospitals would also have to explain how a mother, father, grandmother or grandfather came into the hospital for a hip replacement or other service and died due to contracting COVID-19 in the hospital.
While health care providers have enjoyed some liability protections during the pandemic, many of those protections have now ended and the remaining will end with the ending of the Public Health Emergency. I have no doubt that we will begin to see lawsuits for negligence when patients contract COVID-19 in the hospital and develop complications or die.
To conclude, I suggest reporters consider a few questions for Dr. Sidelinger:
- How will this decision to terminate the rule requiring masks in health care settings make patients safer and protect their health? (It won’t)
- How will ending the requirement to wear masks in health care settings reduce the risks of asymptomatic transmission of SARS-CoV-2 from patients and visitors to staff, from other staff to staff and from staff to patients? (It won’t)
- The rule that is being terminated stated: “Consistent masking by health care providers in health care settings, as well as masking by visitors and patients provides protection to health care providers and to the people they care for. Masks act as source control if the provider has COVID-19 and provide a protective effect if a patient has COVID-19.” Is this information no longer true? (It is still true)
- Is it important to reduce infections with SARS-CoV-2 even if those infections do not cause severe illness or death? (Yes – there remains risk of long-term complications including Long COVID).
- Are there health care workers who are in the high risk category whose health risks would be increased by the end of masking by patients, staff and visitors? (Yes)
- Does infection of immunocompromised persons create a public health risk due to the potential for chronic infection, co-infections, mutations of the SARS-CoV-2 virus and recombinant events that can then enter the general population? (Yes).
- The OHA memo acknowledges that “members of the public, particularly populations at increased risk of severe disease—communities of color, tribal communities, rural communities, lower-income communities, those with underlying medical conditions, seniors, and parents of vulnerable infants” will need the next month to plan their health care visits and protective measures.
- a. It has long been realized, and the pandemic has amplified, that health care disparities exist in the US health care delivery system. Aren’t many of those groups mentioned in the memo as being at increased risk of severe disease and potentially harmed by this decision members of groups most impacted by these health care disparities? (Yes – specifically “communities of color, tribal communities, rural communities and lower-income communities.”) How will this decision not contribute to or worsen these health care disparities?
- b. What planning and additional protective measures other than those these groups are currently doing do you recommend they undertake in order to mitigate the increased risk they will be at from ending the masking requirements in health care settings? The memo specifically points out the planning and protective measures parents should take for vulnerable infants. What additionally can be done to protect a vulnerable infant in the hospital if the staff and visitors are not wearing masks?
There are many steps that can be taken to get to the point where we can eliminate the need for high quality mask use in all health care settings. There is significant research in progress on new vaccines that might confer better mucosal immunity and less transmission of infection. We have learned a lot about improvements we can make to ventilation, air filtration and even air disinfecting measures.
I want to make sure that readers understand that I do not think masks in health care settings are a panacea. They are not. I still see health care workers wearing inadequate respiratory protection like surgical or procedure masks. I still see visitors and some staff wearing masks improperly. However, we must realize that:
- A vaccine only strategy is inadequate, especially in the light of uncontrolled transmission and the development of progressively transmissible and immune evasive variants.
- Perfect need not be the enemy of good, as the saying goes. In other words, even though masks are imperfect, reduction in the amount of virus transmitted can help avoid the development of severe disease.
- We have placed too much emphasis on mortality rates to the exclusion of focus on preventing other complications following acute infection – e.g., MIS-C; MIS-A; cardiovascular, neurological and other complications of infection; and Long COVID (PASC). The avoidance of these complications is also worth our attention and efforts at infection control.
PBS news tonite last wk 2300 deaths and 3000 admissions per day! glenn bothwell
LikeLike
Yes, quite amazing how quickly we can become numb to these numbers. Thanks for pointing this out, Glenn, and thanks for following my blog!
LikeLike
Excellent work and perfect timing, Dr. Pate! I have been so grateful for your dedication to the truth during these three years of the pandemic. I listen faithfully to the Wednesday noon BSU Public Radio Idaho Matters doctors’ roundtable. May you and your wife soon take that long-postponed vacation!
~~Will Browning, Medical Interpreter, Full Circle Health.
LikeLike
Thank you, Will! You have made my day! Thank you for your comment and thanks for following my blog!
LikeLike
I share your very well reasoned concerns, Dr. Pate. It concerns me that politics is trumping medical and public health science.
LikeLike
Thank you, Bill. Yes, before the pandemic, I never would have thought this could have happened. Obviously, I was naïve. Thanks for your comment and thanks for following the blog!
LikeLike
It should be simple. OHA has “a single overarching strategic goal: eliminate health inequities in Oregon by 2030”. Does repealing the mask mandate in healthcare settings move us toward or further away from this goal?
LikeLike
Rachael – an excellent question to add to my list! Thank you and thank you for following my blog!
LikeLike
“The next argument is that this advance notice also ‘gives members of the public, particularly populations at increased risk of severe disease—communities of color, tribal communities, rural communities, lower-income communities, those with underlying medical conditions, seniors, and parents of vulnerable infants – a chance to plan health care visits and protective measures.’”
So, the OHA is basically admitting that these groups of people can expect to suffer harm once masking ends. Get those visits in while you can! Because after that, “Some of you may die, but that is a risk I am willing to take.”
I hate this country, these people, this timeline.
LikeLike
Hi Linae,
Thank you for your comment. I certainly have the same visceral reaction that it appears that you are having, though I think we can strongly disagree and make our disagreement and case for disagreeing clear and objective without hating these people. They may be misguided, inconsiderate, caving to pressure or there may be any number of other reasons for their action, but I certainly can’t place them in the same category as physicians who are purposefully harming people for personal benefit by spreading disinformation, as an example.
Thanks for your comment and for following the blog.
LikeLike