For the past two months, I have been warning of a likely 4th surge of coronavirus cases in Idaho, likely to occur by late March or sometime in April. I have been pleading with our local school districts not to bring back more students to school than can be successfully distanced given the CDC’s prediction that the UK (B.1.1.7 – Kent) variant would be dominant in the US by the end of March. Obviously, it doesn’t make sense to decrease the precautions you are taking when you will be dealing with a new form of the virus that is 40 – 70 percent more contagious, and reportedly causes more severe disease.
It seems that my warnings have largely been ignored and quite surprisingly, one school district decided that my admonitions were inconvenient, leading the board to determine that they would find another adviser who could be more supportive of their plans to bring back all students without proper distancing.
Even more surprising was the fact that the school board never asked me to explain why I was so concerned, nor the even more obvious question, if they were intent on disregarding my warnings: how can we bring all the students back in the safest possible way given the increased risks? I had offered suggestions last fall as to ways we could safely bring back more students and still maintain six feet of distancing, but no one seemed interested, and now it would be much more difficult. Had we done this planning last summer, we likely could have safely had students for full in-person instruction for most of the school year.
So, I thought that I would take this opportunity to explain to my blog followers why I have been predicting this 4th surge, why I think the evidence has only grown stronger over the past two months to support the likelihood of a 4th surge and also refute some of the reasons given by others as to why they don’t believe such a surge will occur.
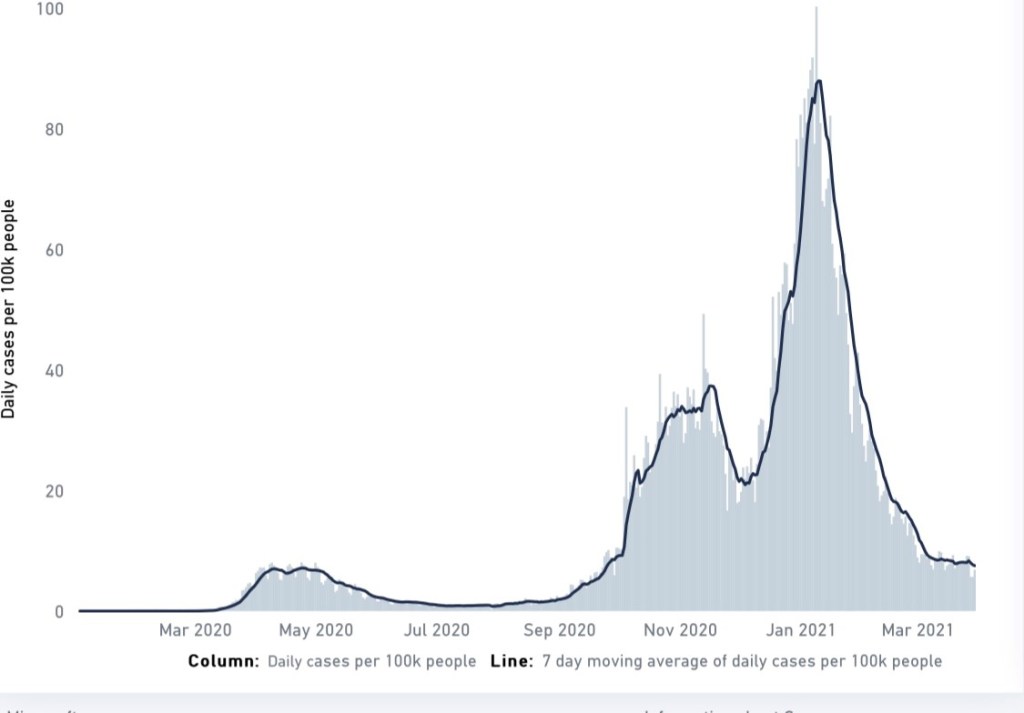
- Let’s start off with looking at the epi curve for the US (see below).
To understand what I mean by a fourth surge, look at the graph. The first surge began on March 12, 2020. The peak of the first surge came on April 9, 2020 with a 7-day moving average of daily new cases of 9.9 per 100,000 population.
Let’s take a moment to give perspective on what these numbers of new cases mean with respect to the degree of disease transmission. People often ask me when we will achieve herd immunity. I don’t know, other than I know it is not going to be April as a well-known physician author wrote recently (see my prior blog piece for an explanation as to why that is completely unrealistic.) However, I am pretty sure we won’t get there in 2021. While everyone wants to know the percentage of the population that has to have immunity to achieve herd immunity (and no one knows the answer to that), I tell them one way to know when we get there is to look at the 7-day moving average of daily new cases. It should be <1 daily new cases per 100k and remain that low for months. We are nowhere near that.
Community spread is when the level of disease transmission in a community is such that we no longer can identify the source of infection. Early on in the pandemic, there was a period of time that we could identify an exposure from travel or an infected person. When we get to the levels of disease transmission associated with community spread, we no longer can reliably pinpoint sources of infection. Using the metric of the 7-day moving average of daily new cases, community spread is 1 – 9 daily new cases per 100k population. So, you can see that at the peak of the first surge, we were at the highest level of community spread.
When the 7-day moving average of daily new cases per 100,000 is in the range of 10 -24, we refer to that as accelerated community spread and when > 25, we refer to that as the tipping point – generally the point where public health experts would call for serious mitigation measures, e.g., stay-at-home orders, closure of certain businesses, etc.

Now, notice something concerning from the epi curve above. We never came down to that well-controlled level of disease transmission of < 1. The lowest point following the first surge occurred on May 28, 2020 when the 7-day moving average of daily new cases per 100,000 was 6.5 – community spread.
We began the second surge from this elevated level of disease transmission. In other words, we loosened up our restrictions too soon. If you recall, people were celebrating the cases coming down, began getting together in larger groups without masks, believing the worst was over, and surely as we moved into the beginning of summer, the virus would go away, though many of us were warning that there was no evidence that there would be seasonality to this virus, and even if there was, it likely would be back in the fall with a vengeance.
So, the second surge was under way at the end of May/beginning of June and peaked July 22, 2020 at a level of 20.3. Notice that this second surge was higher than the first, and like the first, we again did not come down to levels of disease transmission that were under control before we began the third surge. In fact, the lowest point after the second surge was on September 12, 2020 when the 7-day moving average of daily new cases per 100,000 was 10.3. Note that this low point was higher than the low point following the first surge and represented accelerated community spread.
Having this springboard of accelerated community spread resulted in an even higher third surge that peaked January 8, 2021 with an unbelievably high disease transmission rate reflected by a 7-day moving average of daily new cases of 78.3 per 100,000.
Once again, as happened with each of the two prior surges, cases came down from the peak, and I began hearing the all-to-common refrain by now that things were returning to normal (how soon people forget), but coupled by the even more concerning actions by elected leaders across the country to loosen and often terminate all public health measures in place to contain the spread of the virus.
But, while others saw reason to cheer, I became alarmed in the third week of February when I saw the sharp decline begin to plateau, and like the first two surges, at way too high a level of disease transmission – the lower range of accelerated community spread and the higher end of the range for community spread. I had already seen this movie twice and I knew how it turns out.
- So, now let’s look at Idaho’s epi curve:

Idaho, too has experienced three surges, but there are a few differences. Our first case was on March 13 and our first surge peaked on April 4, 2020 at 6.5 average daily new cases per 100,000. But by May 13, we were down to average daily new cases of only 1.3, almost at the containment level. The difference from the US disease transmission was, due to the brave actions of our governor, we had a stay-at-home order in place and it worked. Recall that the U.S. was almost 6 times higher than this level of disease transmission. We know that the governor’s actions saved lives.
Our second surge took off in the middle of June and hit a peak on July 19 at a level of daily new cases of 31.9 per 100,000, higher than the U.S. peak for the second surge. Unfortunately, our low point after the second surge was only 13.4 on September 13. This time, without the stay-at-home order and with COVID-fatigue already setting in, like the rest of the country, Idahoans began relaxing their compliance with public health measures too soon.
Our third surge would begin almost immediately and peaked on December 10 with a 7-day moving average of daily new cases of 91.7 per 100,000. Although cases declined significantly after hitting this peak, as they had in every prior surge, again, I became concerned in mid-February when our state cases hit a plateau and remained in the community spread range, even while many were celebrating a return to normal and our elected leaders were saying all kinds of ridiculous things, like this did not even qualify as a pandemic and there was no longer any need to wear masks, physically distance or restrict the size of gatherings. Of course, in an interesting twist of karma, the legislature then found itself with an outbreak of COVID in the Capitol and as a result had to interrupt the session to recess in order to stop the spread of infection among lawmakers and their staff members — a reminder that we can deny COVID, we can spread lies about it, we can create alternative facts, we can find some doctor out there to tell us what we want to hear that has already been debunked by the medical community, and we can embrace conspiracy theories, but that merely plays into the virus’ hands resulting in many needless infections, as science will always prevail in the end.
While the U.S. and Idaho epi curves explain why I was concerned about a possible fourth surge by mid-to-late February, why was I concerned even before then that we would experience a fourth wave?
There have been two times during the pandemic that we could get a preview of coming attractions. The first was at the beginning of the pandemic in January of 2020 when we could look at the outbreak in Wuhan to see what we might eventually be dealing with in the U.S. – cases of pneumonia that seemed to disproportionately land older people in the hospital. The second time has been since December 2020 in Europe, particularly the U.K., as the B.1.1.7 (Kent) variant quickly evolved over the course of just two to three months to become the dominant strain in the U.S. causing an increase in cases in all age groups and a new surge that was far greater than anything the U.K. previously experienced and was really a surge upon a surge. Let’s look at the U.K. epi curve:
The first surge in the UK peaked on April 24, 2020 at a 7-day moving average of daily new cases of 7.1 per 100,000. But, unlike the U.S., the U.K. successfully brought their disease transmission down to below 1 by July 4, 2020 and it remained low for weeks.
By August 6, 2020, cases began to very slowly rise. Then a sharp rise in cases began at the very beginning of October. At the end of October, the U.K. implemented a lockdown, but allowed schools to remain open. Cases peaked on November 16 at a 7-day moving average of daily new cases of 37.3 per 100,000. By December 4, 2020, cases had come down to a low point of 21. Keep in mind, this level is still in the accelerated community spread level of disease transmission.
But something else was happening under the radar. A new variant had emerged in the U.K. just outside of London in the village of Kent in October. This variant came to be known as B.1.1.7. We saw that it only took 2 – 3 months for B.1.1.7 to become the dominant circulating form of the virus in the U.K. While cases were declining from U.K.’s second surge, the proportion of isolates from people infected that were B.1.1.7 were increasing. What happened next? A new, much larger spike in cases began reaching a new peak on January 10, 2021 with a 7-day moving average of daily new cases of 87.9 per 100,000, despite a lockdown in November and a new lockdown in January. The difference? One difference was that the cases in this most recent, higher spike were mostly B.1.1.7. Another difference was that during the November lockdown, schools were kept open.
The U.K. had previously had the same experience with schools that we had in the U.S. Before the variants, we saw few infections in kids and little spread within schools. So, the U.K. locked down essentially everything but schools at the end of October. However, it soon appeared that the transmission characteristics of B.1.1.7 were different than those of the variant we have dealt with around the world for much of the last year. The U.K. started seeing more infections in children and more outbreaks in schools and daycare. And, lest people think that this was something unique to the Brits, we were also beginning to see the same thing happen in Italy, Germany and Denmark where B.1.1.7 was growing in the percentage of isolates causing infection. Then an interesting fact emerged from the data. While B.1.1.7 tended to increase infections in all age groups, the age group with the highest increase in secondary attack rates (i.e., rates of infection of others who are infected) was 30 – 39-year-olds. Why would that be? In the U.K., adults of that age range should mostly be working from home due to the lockdown. My speculation was that this is likely the age of the parents of children in school. In other words, my concern was that they are having in-school transmission among children, many of those infections might have been mild or asymptomatic and not detected, yet the children were going home from school and infecting their parents.
Obviously, at the beginning of February, we still didn’t have all the answers, but this was enough for me to sound the alarm with our local school districts, but one that fell on deaf ears. As one board member told me as I pleaded with the board not to make a decision in February to bring all children back at the end of March when we knew the best physical distancing we could achieve in schools with students in the hybrid model was 4.5 feet and when I assured them that we would know much more about the variants and how vaccinations were going in Idaho by the end of March: “we don’t care about what might happen then, we are just looking at what is happening today.” I was shocked.
Further myopic was the board and administration’s assessment that things would be fine because children seldom get serious illness and by the end of March, teachers would have had an opportunity to be vaccinated. I tried to point out that students and teachers are not the concern based on what we were seeing in Europe. It is the parents in their 30s and 40s who were not expected to be vaccinated in Idaho by the time they were bringing all students back just as the CDC was predicting that B.1.1.7 would be the dominant circulating form of the virus in the U.S. This didn’t seem to influence them in the least, I presume because they assume that 30- and 40-year-olds don’t get seriously ill. Again, I tried to explain that studies were coming back suggesting that B.1.1.7 was 40 – 70 percent more transmissible and early reports out of the U.K. were that this variant caused more severe illness. I also tried to point out that there are many parents in this age range who have serious underlying health conditions that place them at increased risk, and there are many who are taking chemotherapy for cancer, have immune deficiencies or are taking immunosuppressive medications and may not do well if they become infected with a more transmissible and virulent form of virus. I also tried to point out that some students, especially those in socioeconomically disadvantaged situations may be living in multi-generational households with older family members who may not be vaccinated, and will be at very high risk due to age and potentially underlying medical conditions. It was if I was talking to myself.
By this time, it was not only the UK, but Italy, Germany, and Denmark that would give the world warnings that B.1.1.7 transmission characteristics were different. While children did not seem to get sick as often as adults and did not seem to spread infection within schools or contribute to community spread prior to the rise in B.1.1.7, the countries and others were now indicating that there seemed to be significant spread in schools that was contributing to community spread and these countries were now closing schools. They warned the world that B.1.1.7 is more transmissible, causes more severe disease and that it is much more difficult to contain its spread. The U.K. warned that maintaining physical distance was the only hope to controlling the spread of this variant.
So, for all these reasons, I was very concerned that this was exactly what would happen in the U.S. Why would we be different? Some dismissed my concerns believing that what happens in Europe has no bearing on what will happen in the U.S., let along Idaho. Then it started happening in Canada. That still did not persuade people. But, recently, it started happening in the U.S. While I had hoped that I was wrong and overreacting, all the evidence kept affirming my fears. So, let’s look at a few examples of this additional evidence.
- Outbreak of B.1.1.7 infections in Minnesota in late January into February 2021. From the Minnesota Department of Health – Since late January, at least 84 cases of COVID-19 have been linked to participants in both school-sponsored and club sports activities, including hockey, wrestling, basketball, alpine skiing, and other sports. In addition, health officials have seen increases in cases in Carver County gyms and fitness centers, with many of the cases linked to the sports-related cases. The Minnesota Department of Health (MDH) has observed a concerning increase in the rate of growth of cases in Carver County over the past month (a 62% increase between the week beginning Jan. 27 to the week beginning Feb. 24). Case rates in Carver County are now approaching rates seen in October 2020, and a high proportion (35%) are under age 20.
“We are increasingly concerned about dramatic increases in cases, particularly in Carver County where the B117 variant has been confirmed.”
Through recently completed whole genome sequencing of a portion of the sample specimens from the outbreak cases, health officials confirmed 27 cases of the B117 variant, a highly contagious and potentially more virulent variant first identified in the United Kingdom. Cases have occurred in athletes, coaches, students, and household contacts. Multiple schools, both public and private, have confirmed cases tied to the variant strain cases. Many of the people with B117 variant COVID-19 attended school or sports activities while infectious. The concern is this highly contagious variant has the potential to spread exponentially and quickly across youth who are largely unprotected by vaccines.
- In one week in early March, Duke University had an outbreak of COVID cases among students. The number of new cases in that one week exceeded the total number of cases that occurred during the entire Fall semester.
- We have seen a large outbreak of new COVID cases in Eastern Idaho. Looking at just one of the involved counties, Bonneville, the peak occurred on March 14 and reached a 7-day rolling average of daily new cases of 72.8 per 100,000.
- Although we do not do enough sequencing in the United States or in Idaho to know what percent of cases are currently caused by B.1.1.7, we do know that B.1.1.7 is significantly increasing and has become the most frequently identified variant of concern in samples that are sequenced. European countries have warned that once B.1.1.7 surpasses accounting for half of the circulating virus, we can expect a soon upcoming surge.
- The testing positivity rate in Idaho had fallen to 4.5% by the third week of February, but has increased to 5.5% by mid-March.
- What is happening now?
- New cases in the U.S. are up 20% from the prior two weeks.
- Cases are in the accelerated community spread category, increasing and staying high in 28 states plus the Virgin Islands and Washington D.C.
- Deaths are increasing in 8 states plus Washington D.C.
I could keep on going with examples, but let’s look at one more local indicator that I find fascinating.
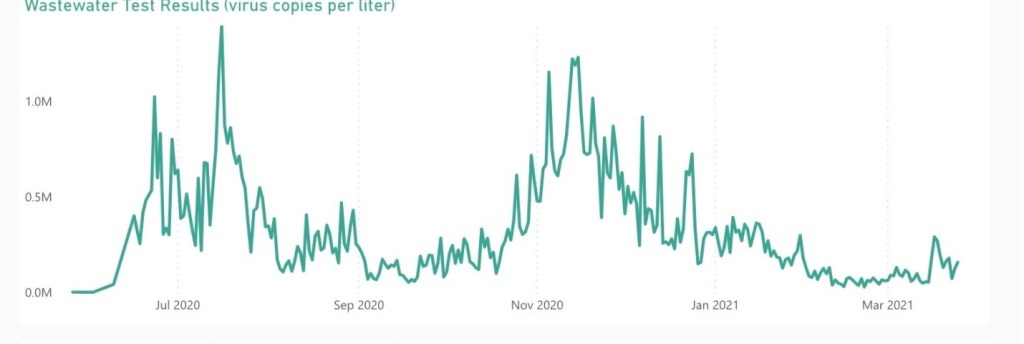
This is the wastewater testing for SARS-CoV-2 virus done by the City of Boise. It shows that we got to a low on February 14 of about 33,000 virus copies per liter, but it has been increasing since then, signifying more virus (i.e., more infections). By March 17 it had peaked at about 293,000 virus copies per liter. As of the last date of data available (March 25) the count was about 160,500, i.e., almost a 5-fold increase in viral levels from the low just the month before.
So, I will stop here and address some of the counter-arguments. But, hopefully you can get a sense of why I have been predicting this upcoming 4th surge.
Arguments:
- The vaccine roll-out will stem this surge. My response – I hope so, but don’t think so. We simply do not have enough people vaccinated to get us anywhere near herd immunity. For more on this, see my prior blog piece.
- We don’t have to worry about Boise or West Ada schools because the CDC said we can operate schools safely with only 3 feet of distancing. Response – Wrong. The CDC has indicated that 3 feet of distancing is not recommended for schools in communities with the highest levels of disease transmission (which is what the CDC considers Ada County to be in) and the CDC indicated that in all cases there should always be at least 6 feet of distancing when students have masks off (for example, the cafeteria), but in all the schools I inspected, I never found a school that could get more than 4.5 feet of distancing in the cafeteria with only half the students in attendance.
- We have been able to prevent transmission among health care workers in hospitals where they often work less than 3 feet apart. Response – Two big differences. First, the majority of health care workers have been vaccinated. Almost no children have been vaccinated. Second, this was the experience with the wild-type virus, not B.1.1.7. In fact, one of the Duke hospitals just reported an outbreak of COVID cases on a cancer unit involving 20 staff and patients.
- We don’t have to be concerned because it has warmed up and everyone will be outside and so we won’t have much spread of the virus. Response – (1) There is absolutely no evidence of seasonality of this virus. (2) Why do you think that will be the case this year when it wasn’t last year? Note from the epi curves for the US and Idaho above that the surges in the summer were far greater than the first surges in March/April of last year. People don’t spend all day, every day during the warmer months outside. In fact, in many places in the country, the heat and humidity cause people to move indoors during the middle of the day for air conditioning.
Well, we will know soon enough who is correct. I pray that I am wrong, but as I review the activity around the world and in the U.S. and even here in Idaho, I only become more and more convinced that I am right. We will know soon enough.
Thank you Dr. Pate for your very thorough and fact based analysis of the Covid virus impact this past year and what we may face moving forward. It is surprising to me that, especially in the school system, these facts are ignored despite what best serves students and the community. Your passion for healthcare is obvious and your warnings should be heeded. Sadly, severe illness or loss of life may be the only result that will wake people up to continue diligence with mask wearing and social distancing.
LikeLike
Thank you, Dotty! Yes, it has been very disappointing to see so many people in positions of leadership not put science and the interests of those they serve ahead of other personal or political benefits. I hope you are well! Thanks for following my blog!
LikeLike
Dear Dr. Pate, Thank you very much for your well documented and cogent blog posts. I also greatly appreciate that you clarify what the public health community does not fully understand about COVID-19 and its various mutations. I believe you and NOT Dr. Makary! I have made a decision (at least for now) not to get my second dose of Moderna based on some rather new research/thinking about the high efficacy of the 1st dose, and what I’ve read about the nature of immunity build-up over the course of several months. This editorial in the NEJM caught my attention: NEJM https://www.nejm.org/doi/full/10.1056/NEJMc2036242. I am scared of the 2nd dose side effects that some of my friends have experienced. I figure the 2nd dose has negligible benefit and that I am at a relatively low risk otherwise (healthy 55 year old who works at home and always wears a mask in public). Plus someone else can benefit from my unused vaccine for their 1st dose. I also figure that I’d rather get a booster next year when there might be improved vaccine protection against these variants. Do you think there is enough validation in the scientific literature to support my decision not to get the 2nd dose of Moderna?
LikeLike
Hi Alyssa. I completely understand how you came to your decision and the basis for it based on the information you cited. However, that is not the full story. Three reasons that you should go ahead and get the second dose. (1) In testing sera from people who have had one or two doses of vaccines against the variants, a single dose of vaccine, though still very high effectiveness against the wild-type virus and the UK variant (as you referenced), gave almost no protection against the South African variant. People did not show any significant neutralizing antibody levels against the South African strain until after the second shot. (2) [note – this one is very complicated, so I am going to oversimplify it] Though we don’t have detailed studies on this yet, we think that the first shot is most important for stimulating the humoral part of the immune system (antibodies), but the second shot is important for stimulating the cellular immune system (these are the cells that are critical to killing the virus once it gets into your cells because antibodies can’t get inside your cells). The second shot is also probably very important for what we call durability – i.e., how long your immunity will last. (3) Finally, we have at least 5 variants of concern circulating in the U.S. right now. The second shot will boost your neutralizing antibody levels up to high enough levels that you will have protection against some of the variants with immune escape capabilities. So, I understand your thinking, but PLEASE, get the second dose! I did. And, I had a rough day after, but much better than having COVID! I will happily get a booster next year, if needed.
LikeLike
Thank you Dr. Pate. Your response to my question was amazing and I will certainly get the 2nd dose now that I more fully understand why it is necessary. I don’t know how anyone can possibly disagree with your interpretation of the scientific literature as it is clear you read everything and have a deeper understanding of the coronavirus than anyone else. I apologize for digressing (with my personal matter) from the main theme of your extremely important article about a bigger fourth wave of infections driven by young people. There is no doubt in my mind that you are right about the need to close schools now.
LikeLike
I am so pleased that you will get the second shot. And, never apologize for asking questions. I am glad you did.
LikeLike
Thank you Dr Pate for the science and epi based facts regarding the rolling case rates over time. It’s clear that now is not the time to relax preventive measures regarding community spread of Covid 19 and its variants. Get vaccinated, mask up, keep safe distances, and wash your hands often.
LikeLike
Thank you Dr. Pate for all your work and this detailed analysis. I too fear you are correct in your projection of the fourth wave. Why we as a society seem intent on learning the hard way is perplexing to me, along with shy so many of our citizens view the pandemic and our response as a political rather than a public health issue.
LikeLike
Thank you! Yes, it has been frustrating. It seems many of us need to learn the hard way. Thanks for following the blog!
LikeLike
Well said! Thanks, Jim! And, thanks for following my blog!
LikeLike
David, I have great respect for your knowledge, experience, and analysis, but I don’t agree that schools should be closed. As we all know, it’s not a risk-free world, and I believe keeping kids at home all these months has brought problems that far outweigh the risks of having schools open. Our children will be bearing the scars of this episode long after adults have gone on their way.
Best—
Alice
>
LikeLike
Hi Alice. I think you misunderstand my position. I actually agree with you.
Here are my points:
1. We could have had full, in-person instruction all year long with some advanced planning and done it safely. We knew last Spring at the onset of this pandemic that it would likely impact the entire upcoming school year. Unfortunately, WASD didn’t engage me until October when they were in crisis – teachers were threatening a sick-out and parents were staging protests. Unfortunately, at that point, the WASD plan approved by CDH had been to go full remote, so I had to spend countless hours working on an operational plan with administration and CDH so that we could at least operate in hybrid. I wanted kids in school if we could do so safely and we did. But, I threw out ideas for how we could bring back kids for full, in-person instruction and still keep them distanced, likely using some of the federal funding that was going to schools, but there was no interest in pursuing these ideas. Had we had these discussions over the summer, perhaps we could have made these preparations. A university in another state had implemented these ideas with great success.
2. At this point, this late in the school year, it probably makes little sense to make these investments now – we missed the opportunity. So, I begged them to keep kids in hybrid rather than bringing everyone back when we knew that the best distancing we could achieve even in hybrid was 4.5 feet. My point was that if you look at how much different the UK variant is in children and the bigger role they play in transmission than they played before, if we bring everyone back with less than 3 feet of distancing, we are almost certain to have school-wide outbreaks that will force us to send all kids to full remote. My point was that it seemed to me better to at least have kids in-person half-time than all kids home for full remote.
3. I don’t disagree with the fact that damage has been done to kids this year. But, that is due to poor planning. I can’t fix that now. As you know, I am not an education expert. My guess is that attendance for two months (and I really will be surprised if Boise and West Ada schools can stay open more than a month with the reports I am getting as to what is happening in schools) is not going to reverse the damage done. If I am wrong, then perhaps the risks are worth it. I really don’t want to be an alarmist, but I don’t think people understand how bad things are going to be within the next few weeks, and how much different things are going to be than what we saw before. If you talk to those in areas where they have already had the surge of this new variant, they can better describe what we will see with young adults critically ill in hospitals – especially, the parents of these school children. This fourth surge is very likely to be bigger than the surge we just came off of. There are worse things than the educational gap we are going to have to fill; things that will also scar these children, but for which there is no hope for undoing or repairing. Frankly, at this point, it would have just been better for schools to close now for the spring break and not resume school until the summer when we can get past this threat and kids could be safely be returned for full in-person education for the entire summer to being the work of catching up.
If I am wrong, I will gladly accept the blame and no one need listen to anything I say about this again. But, I haven’t heard one other person in Idaho giving these warnings and yet I am more certain of this prediction than anything I have opined on for the past year. I sincerely pray that I am wrong. I will take no pleasure in being right, because it will come at a tremendous cost to Idahoans. But, if I am right, and with no one else speaking out (I do believe there are others out there that share my predictions, but they are too afraid to say so publicly, because if it doesn’t materialize, they know they will be criticized for fear-mongering and overreacting), I feel that I have to warn people strongly and loudly to protect themselves. I would not be able to live with myself if I remained quiet.
LikeLike
Alice,
I can’t believe it. Right after I finished writing the above response to your comment, I went to read updates on the coronavirus. Here was the first article I turned to. It is from Medscape:
Public health officials in the Midwest and Northeast are sounding the alarm about steep new increases in COVID-19 cases in children.
The increases seem to be driven by greater circulation of more contagious variants, just as children and teens have returned to in-person activities like sports, parties, and classes.
“I can just tell you from my 46 years in the business, I’ve never seen dynamic transmission in kids like we’re seeing right now, younger kids,” said Michael Osterholm, PhD, who directs the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis.
In earlier surges, children — especially younger children — played only minor roles in transmitting the infection. When they were diagnosed with COVID-19, their symptoms tended to be mild or even absent, and for reasons that aren’t well understood, they haven’t usually been the first cases in households or clusters.
Now, as more SARS-CoV-2 variants have begun to dominate, and seniors gain protection from vaccines, that pattern may be changing. Infectious disease experts are watching to see if COVID-19 will start to spread in a pattern more similar to influenza, with children becoming infected first and bringing the infection home to their parents.
Michigan Sees Jump in Cases
Governors in some hard-hit states are pleading with a pandemic-weary public to keep up mask-wearing and social distancing and avoid unnecessary travel and large gatherings in order to protect in-person classes.
In Michigan, many schools reopened and youth sports resumed just as the more contagious B.1.1.7 variant spread widely. There, cases are rising among all age groups, but the largest number of new COVID-19 cases is among children ages 10-19, the first time that’s happened since the start of the pandemic.
Over the past month, incidence in this age group has more than doubled in the state. Cases among younger children — infants through 9-year-olds — are also going up, increasing by more than 230% since February 19, according to data from the Michigan Department of Health and Human Services.
The increases have prompted some schools to pause in-person learning for a time after spring break to slow transmission, according to Natasha Bagdasarian, MD, senior public health physician with the Michigan health department in Ann Arbor.
In Minnesota, on a recent call with reporters, Ruth Lynfield, MD, state epidemiologist, said the B.1.1.7 variant, which has rapidly risen in the state, has a higher attack rate among children than earlier versions of the virus, meaning they’re more likely to be infected when exposed.
LikeLike
You are likely correct.
LikeLike
David, this was fascinating. Thank you for providing the data to prove your position. I am sorry the school districts are not listening to you. They should for the sake of the children and their parents.
LikeLike
To what extent do you think kids should be protected from covid, especially once all adults have had the option to be vaccinated? I have a one year old who won’t be eligible to be vaccinated for quite some time. So far, we’ve been very careful his entire life (grocery pickup only, work from home and don’t use childcare, only see people who have quarantined, etc). Soon, my husband and I will be fully vaccinated. We plan to get together with other vaccinated adults. But, I’m not sure what to do about kids. Should we let him interact with other kids who aren’t quarantined or vaccinated? Sounds we take him to the grocery store? I’m a stay at home parent and my husband works from home and we have no other kids. So, we have the luxury if being able to keep him in a bubble indefinitely- but to what extent do you think that’s even necessary?
LikeLike
Hi Heidi,
It is a great question and one that is very difficult to answer. That is because, while children seldom get severely ill or die from COVID, we are learning more and more about the long-term effects of even mild infection in not an unsubstantial percentage of kids (perhaps around 10%?) who get infected. Therefore, I think it reasonable to take some precautions, but if your child is otherwise healthy, I don’t see a need to go to extremes. For example, I would not have significant concerns about your child playing outdoors with another child whose parents are vaccinated. I also would not have concerns about having some vaccinated friends or family over to the house and being around your child. On the other hand, I don’t know that I would take a child to a large gathering where people will be huddled together, especially if indoors. I also don’t think I would travel with him at this time since he is too young to effectively wear a mask.
The good news is that I do think it very possible that we may have vaccines authorized for children his age this fall or at least by the beginning of the next year. Thanks for following the blog!
LikeLike
Dr. Pate, wondering if we can get your take on the new CDC guidance regarding masks, and where we might be headed as a community and country this summer. I’m also very interested in your thoughts around the “haves and have nots” when it comes to international access to vaccines, and how that may impact the United States in the long term. In short, is it in our national self-interest to use our wealth to ensure vaccinations get to all corners of the planet? Thanks for the time that you put into producing these blog entries!
LikeLike
Scott,
Excellent questions. I answered some of them in a new blog post just this morning. I hope you enjoy, and please ask more questions that the post does not answer. You bring up an important point. Pandemics are interconnected, world-wide challenges. No country will be safe if it only vaccinates its own citizens. Take care, be safe and thank you for following my blog!
LikeLike